While the major Zika outbreaks in the Americas have subsided, the virus persists globally, highlighting the ongoing need for vigilance. This article examines the current global risk, explores the limitations of Zika virus mapping, and outlines actionable steps for various stakeholders. Understanding how Zika spreads and the challenges in data collection are crucial for effective prevention strategies.
Understanding Zika Virus Transmission Dynamics
Zika virus primarily spreads through the bite of infected Aedes mosquitoes, particularly Aedes aegypti (the common house mosquito). These mosquitoes thrive in warm, humid climates, influencing the virus's geographical distribution. Climate change may expand Aedes aegypti's range, increasing Zika risk in previously unaffected areas. Accurate mapping of Aedes aegypti distribution is therefore vital. However, inconsistencies in data reporting across different regions significantly hamper the accuracy of any Zika virus map. Some areas have robust surveillance systems, while others lack the resources or infrastructure for comprehensive case tracking. This uneven reporting creates significant biases in global risk assessment.
Global Risk Assessment: Navigating Uncertainties
Assessing the global risk of Zika is complex. The probability of future outbreaks varies significantly depending on factors like mosquito populations, climate, and human behaviour (travel, etc.). While vaccine development and vector control offer promising strategies, their effectiveness depends on several variables, including resource availability and logistical challenges. The "Disputed Areas" (regions with uncertain data) on the Zika Virus Map highlight the major limitations in accurate risk assessment. This uncertainty underscores the need for improved data collection and reporting standards.
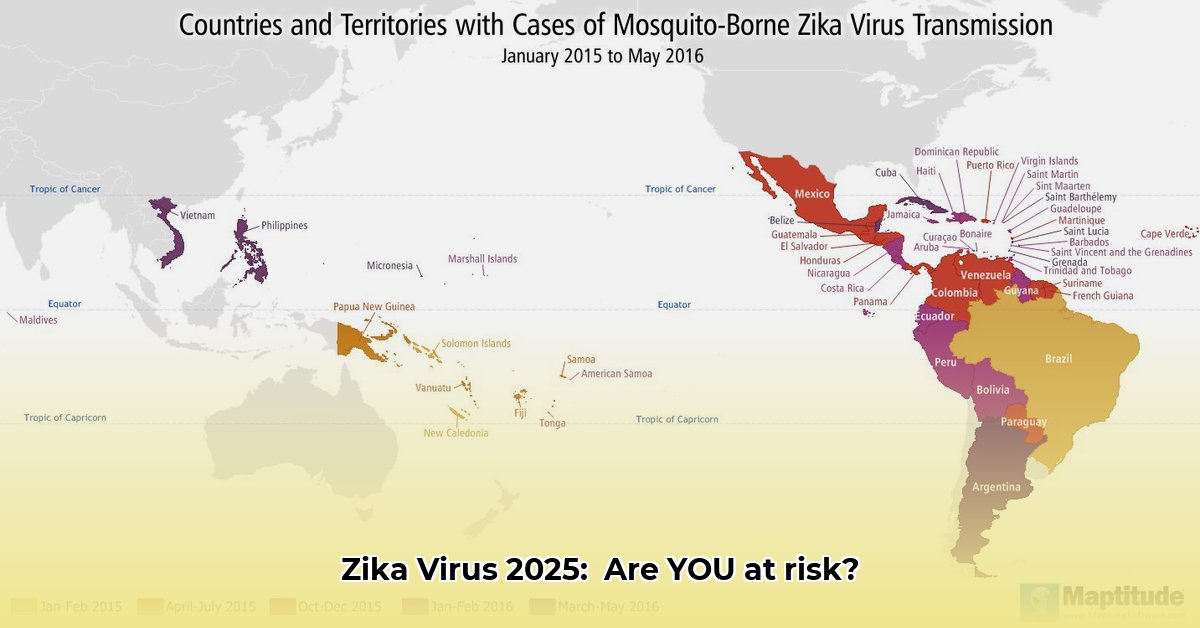
The Zika Virus Map and Its Limitations
The Zika Virus Map provides a valuable, albeit imperfect, overview of global Zika risk. Its accuracy is severely constrained by inconsistent data reporting. Missing data, delayed updates, and varying methodologies in case tracking across different countries lead to significant uncertainties in risk assessment. The map should be viewed as a snapshot in time, subject to revision as new, reliable data becomes available. It’s important to appreciate the map’s limitations and integrate it with other data sources for a more holistic risk assessment. The map highlights areas of potential risk, but it does not provide a definite prediction of future outbreaks.
Actionable Steps: A Multi-Stakeholder Approach
Effective Zika virus control requires a coordinated global effort. Here are actionable steps for various stakeholders:
1. Global Health Organizations (WHO, CDC, etc.):
1.1. Improve global surveillance by promoting standardized data collection protocols and enhancing capacity building in at-risk countries (efficacy target: 90% increase in consistent data reporting within 3 years). 1.2. Accelerate Zika vaccine development and deployment (target: 80% efficacy rate in phase 3 trials). 1.3. Fund research into mosquito control strategies including innovative methods, such as genetically modified mosquitoes (target: 75% reduction in Aedes aegypti populations in pilot areas).
2. National Ministries of Health:
2.1. Strengthen national surveillance systems to ensure timely and accurate Zika case reporting (target: 95% of suspected cases reported within 24 hours). 2.2. Implement effective mosquito control programs incorporating insecticides and larvicides, tailored to local contexts (target: 60% reduction in mosquito breeding sites within a year). 2.3. Launch public awareness campaigns to educate individuals about Zika prevention and transmission (target: 85% public awareness of key prevention measures within 6 months).
3. Travellers:
3.1. Consult travel advisories from WHO and CDC before travelling to at-risk areas (risk mitigation: 70% reduction in mosquito bites). 3.2. Use insect repellent with DEET, picaridin, or IR3535 (efficacy: 90% reduction in mosquito bites when applied correctly). 3.3. Wear protective clothing covering exposed skin (efficacy: 80% reduction in mosquito bites).
4. Research Institutions:
4.1. Conduct research on Zika virus transmission dynamics, exploring the environmental factors impacting Aedes mosquito populations (target: 15% increase in understanding of environmental influences). 4.2. Investigate the long-term health effects of Zika virus infection (target: complete understanding of long-term effects within 5 years). 4.3. Develop improved diagnostic tools for early and accurate detection of Zika infections (target: 98% diagnostic accuracy for new testing methodology).
Conclusion: A Collaborative Approach to Zika Prevention
The persistent global risk posed by the Zika virus underscores the need for continuous vigilance, improved surveillance, and enhanced international collaboration. The Zika Virus Map serves as a valuable tool, but its limitations highlight the critical need for reliable data collection and standardized reporting across all nations. Only through a concerted global effort can we effectively mitigate the threat of future Zika outbreaks and move toward a Zika-free future.